Tech advances in healthcare have benefited millions. From online doctor appointments to remote diagnosis aides like the digital stethoscope, digitalized medicine and telehealth has increased health access for many.
But some groups are locked out of healthcare despite the digital healthcare revolution. Hospitals and clinics, and medical device developers and suppliers must be more aware that a good portion of the population can’t use some new services, because their needs weren’t considered in the design. I’m talking about the 15 percent of the global population with a disability – from learning disability to visual impairment to motor impairments and many other conditions. If people with disabilities can use these new technologies, they could benefit more than any other group.
Accessible health tech doesn’t happen by accident
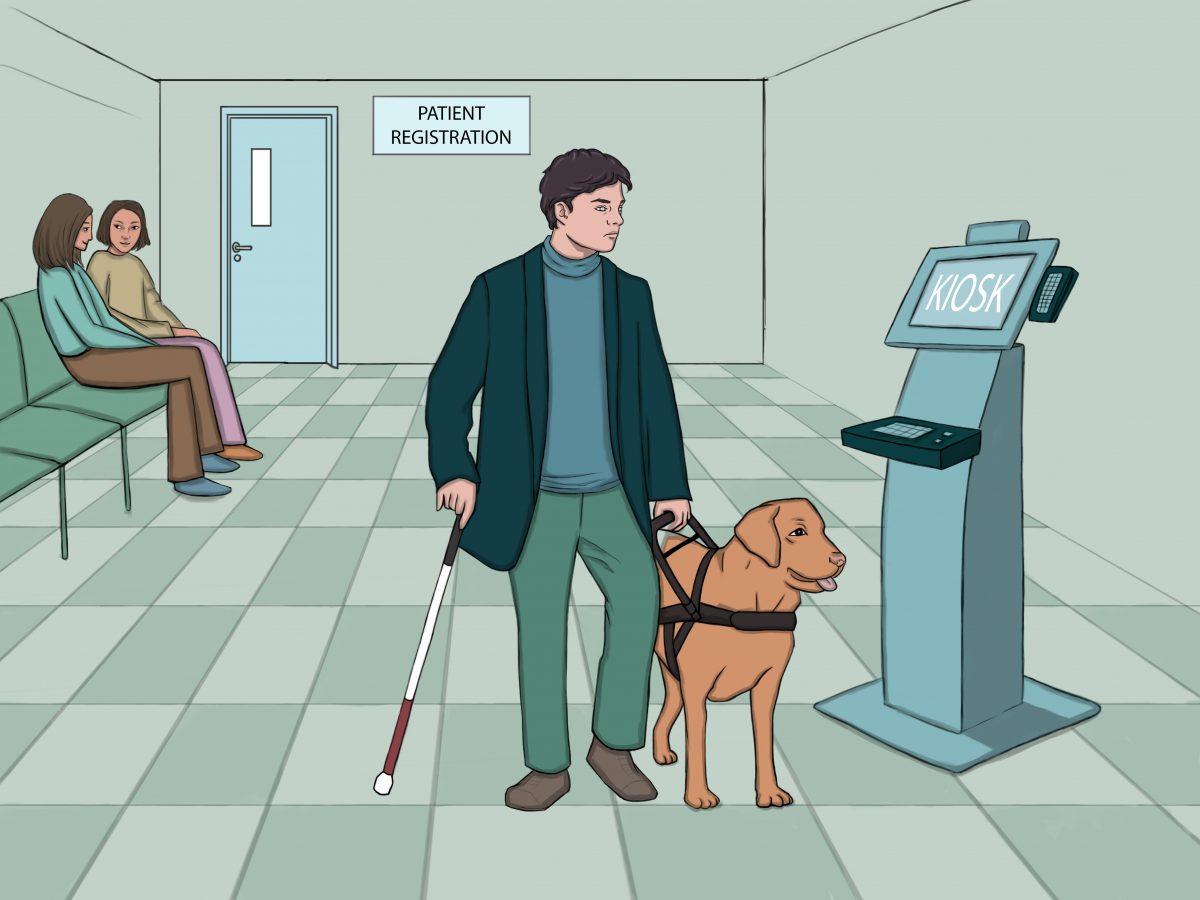
Imagine you’re blind and have a chronic health condition, so you need ongoing doctor appointments. You’ll be expected to organize much of this online, including registering on the clinic’s portal, booking appointments and paying bills. If your appointment is in person, you may need to check in using an automated kiosk or speak to your doctor online using video conferencing.

Kaspersky Healthcare Cybersecurity
Health cybersecurity
Today’s healthcare needs fighting fit cybersecurity.
While these tasks are effortless for many people, they can be a barrier for those with disabilities. Cutting-edge technology too often leaves the most vulnerable behind.
Medical devices should be tested with customers with a range of disabilities to make sure they can use them. Still, studies show patients with disabilities report many problems using medical devices and equipment. When accessibility is considered, it’s often an afterthought rather than a requirement.
Around the world, many countries have laws safeguarding the rights of people with disabilities. Ignoring these regulations is a risk for business and public institutions alike. Digital accessibility lawsuits are fast increasing.
Examples of accessibility barriers in health tech
Blood glucose meters
Blood glucose meters or glucometers help people with diabetes track blood sugar levels to ensure they stay within a healthy range, usually by the user placing a drop of blood on a testing strip and reading the blood sugar level from a screen.
That’s easy unless you have, say, a tremor, lack of dexterity or low vision. Diabetes can cause sight loss, making impaired vision more common among people with the condition.
Inaccessible equipment may force some diabetics to rely on others to help keep their conditions in check. This loss of independence can be frustrating: Relying on others may mean scheduling your life around them or extra costs for rides or aides.
Pregnancy tests
For many, a pregnancy test result is something they want to share with a partner or other people, but not always. What if you couldn’t see the result and had to ask someone to read it for you? UK charity supporting those with sight loss RNIB has developed a prototype for a tactile pregnancy test which may one day be a mainstream product.
Appointment check-in kiosks
Nowadays, institutions and businesses offer digital kiosks for many tasks, like checking in for flights and ordering food. In healthcare, kiosks are especially popular for appointment check-ins.
Most kiosks rely on physical touch and being able to see a screen. There are ways to make them more accessible, like using Braille and large print for labels, having audio jacks for speech direction and making sure the height suits wheelchair users.
Protecting patient privacy is critical. More accessible kiosks would help people with disabilities maintain privacy while providing information a healthcare institution might need.
Laura Miller, former co-chair of the kiosk accessibility committee for the Kiosk Manufacturers Association, says, “Without access to medical information, autonomy in viewing and updating personal healthcare facts and the right to medical record privacy, people with disabilities can’t securely navigate their medical journey without help. Critical to an accessible healthcare experience is being able to privately listen thanks to a headphone jack and screen reader and being able to navigate and communicate information.”
Website and app accessibility
A visually impaired patient may need to use different websites and online portals for healthcare-related tasks, like using review sites to research doctors or using online portals to get medical records. If these websites are not accessible, they would have to ask someone for help.
To a visually impaired person using a screen reader (software visually impaired web users use to read out web content), inaccessible websites can seem like the aftermath of a Black Friday sale: Jumbled content all over the place. When they’re told a link is labelled “click here,” how could they know where it will lead?
Keyboard-only users (not everyone can use a mouse) may find it impossible to fill out a form or reveal roll-over content. A cognitively impaired person may be overwhelmed by huge blocks of text not broken up by headers. Someone with low vision or color blindness may not be able to see buttons or read text that contrasts poorly with background color.
There are guidelines to follow to make websites, apps and PDF forms accessible. The World Wide Web Consortium (W3C) – an international organization seeking universal web access – developed the Web Content Accessibility Guidelines (WCAG) in consultation with disabled web users. These guidelines give technical criteria that make the web easier to use for people with many impairments. For example, using descriptive link text ensures those using a screen reader can understand where a link will lead them. Making calls to action and navigation links larger helps someone with reduced dexterity more easily use them.
Although many of these guidelines are easy to follow when you know how, most websites don’t follow basic web content accessibility guidelines.
Online medical appointments
Online appointments, sometimes called telehealth, skyrocketed during the pandemic. Though it won’t replace in-person doctor visits, it’s convenient and cost-effective, and many have chosen to keep using the service. It’s even more important that people with disabilities can access online appointments because some face barriers leaving their homes, making in-person appointments hard.
But if the remote appointment app or website doesn’t work with screen readers, visually impaired people may not be able to use it without help. Telehealth is off the table for patients with a hearing impairment unless there are on-screen captions (subtitles.)
How to start your accessibility journey
What every company or organization must do to improve accessibility for patients, customers and clients is different, but here are some ways to get started.
Automated accessibility testing
A fast way to understand your digital content’s accessibility is to run an automated scan for machine-detectable accessibility errors using a tool like ARC Monitoring. Google Lighthouse also has accessibility assessments among its features.
Automated scanning identifies less than half of the barriers a person with disabilities may encounter online. You must manually audit to make sure you catch all problems.
Manual accessibility auditing
An accessibility audit is a manual review by an expert that finds WCAG failures only a human can identify. While any trained accessibility auditor should know the difference between accessibility ‘box-ticking’ and true accessibility, organizations like TPGi and Australia’s Disability Accessibility Centre have auditors with the disabilities they’re checking for barriers around, so could give you a more reliable and thorough picture.
Ask for feedback
While it’s best to get feedback on a product or digital application during design and build, it’s never too late to find out what users think. Ask for feedback from people with disabilities on where they’re finding barriers, for example, by providing an accessible online form, email address or phone number for reporting an access barrier.
Focus on the most crucial user journeys – the main things your users need your service to do. Observing users trying to get through these journeys, either in person or remotely, can be hugely informative.
Bear in mind, voluntary feedback isn’t enough to ensure a product is accessible. Not all customers want to or have time to tell you about barriers they face.
Once your tech is accessible, maintain it
Once your organization is at the point where its tech is reasonably accessible, you need to maintain the accessibility. Here’s how.
Decide accessibility is a must for every project
Buy-in from stakeholders matters. Projects may need longer timelines for more quality assurance, developers may need training and it may cost more to ensure you’re doing it right. Buy-in from senior leadership affects everything the organization does, from the culture to choosing vendors to your results.
Build accessibility into product and service design
The earlier in the design process you consider accessibility, the better. Your website is probably the biggest product you control, so if you’re planning a redesign or adding something new, bake in accessibility considerations. You’ll save time on a smoother launch and fewer remediations down the line.
Monitor accessibility
Digital assets are always changing. As you update websites and add new content, monitor for accessibility issues.
Train employees in accessibility
When you train employees in all divisions, not just developers, on what accessibility is and why it matters, it creates an inclusive culture. People start adding accessible features, code and tactics to projects, meaning better results and fewer fixes later.
It may seem daunting to start an accessibility journey, but the rewards outweigh the obstacles. People with disabilities could gain much from healthcare’s digital transformation, but tech designers must make sure we understand and commit to accessibility. There’ll always be more to learn, but with forethought, we can design healthcare tech that meets more people’s needs.



